Sang Eun Lee,1 Seung-Ju Lee,1 Song-Ee Kim,1 Kinam Kim,2 Boyoung Cho,2 Kyounghwan Roh,3 and Soo-Chan Kim4
Published January 25, 2021 – More info
BACKGROUND. Recessive dystrophic epidermolysis bullosa (RDEB) is an incurable disease that causes severe mucocutaneous fragility due to mutations in COL7A1 (encoding type VII collagen [C7]). In this phase I/IIa trial, we evaluated the safety and possible clinical efficacy of intravenous infusion of allogeneic human umbilical cord blood–derived mesenchymal stem cells (hUCB-MSCs) in patients with RDEB.
METHODS. Four adult and two pediatric patients with RDEB were treated with 3 intravenous injections of hUCB-MSCs (1 × 106 to 3 × 106 cells/kg) every 2 weeks and followed up for 8–24 months after treatment. The primary endpoint was safety. Secondary endpoints related to efficacy included clinical parameters, such as disease severity score, wound assessment, itch and pain score, and quality of life. C7 expression levels and inflammatory infiltrates in the skin, as well as serum levels of inflammatory markers and neuropeptides, were also assessed.
RESULTS. Intravenous hUCB-MSC infusions were well tolerated, without serious adverse events. Improvements in the Birmingham Epidermolysis Bullosa Severity Score, body surface area involvement, blister counts, pain, pruritus, and quality of life were observed with maximal effects at 56–112 days after treatment. hUCB-MSC administration induced M2 macrophage polarization and reduced mast cell infiltration in RDEB skin. Serum levels of substance P were decreased after therapy. Increased C7 expression was observed at the dermoepidermal junction in 1 of 6 patients at day 56.
CONCLUSION. To the best of our knowledge, this is the first clinical trial of systemic administration of allogeneic hUCB-MSCs in patients with RDEB, demonstrating safety and transient clinical benefits.
TRIAL REGISTRATION. ClinicalTrials.gov NCT04520022.
FUNDING. This work was supported by Daewoong Pharmaceutical Co. Ltd. and Kangstem Biotech Co. Ltd.
Epidermolysis bullosa (EB) is a group of genetic diseases characterized by mechanical fragility of skin and mucosa (1). Recessive dystrophic EB (RDEB) is caused by mutations in COL7A1, which encodes type VII collagen (C7), the main constituent of anchoring fibrils at the dermoepidermal junction (DEJ). RDEB is one of the most severe forms of EB; it is characterized by recurrent blistering, chronic wounds, disabling scarring in the skin, and mucosa and internal organ dysfunctions, leading to substantial morbidity and mortality (2–4). Currently, there is no cure for this severe subtype of EB; however, novel therapeutic strategies have been developed in the fields of gene and cell therapies (5–15).
Mesenchymal stem cells (MSCs) have been identified as an attractive option for allogeneic cell therapy for RDEB based on their potential mechanisms of action, including immunomodulation, migration to damaged tissue, stimulation of tissue regeneration, and reduction of fibrosis, mainly through paracrine activities (8–11, 14–16). Locally injected allogeneic bone marrow–derived MSCs (BM-MSCs) have shown to accelerate wound healing, with transient C7 restoration in patients with RDEB and a mouse model of dystrophic EB (10). Two early-phase clinical trials of systemic administration of allogeneic BM-MSCs in 23 pediatric patients with RDEB reported variable clinical benefits that lasted for several months with satisfactory safety (8, 9). An additional recently published phase I/II trial of intravenous BM-MSC injection in 10 adult patients with RDEB also showed transient, but clinically meaningful, improvements in disease severity, skin inflammation, and pruritus, with no serious adverse events (AEs) (14).
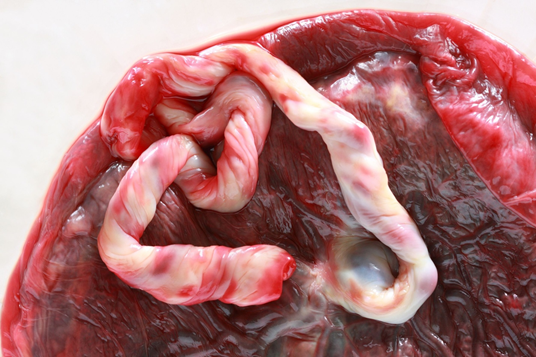
To our knowledge, previous clinical trials for RDEB have examined the potential of BM-MSCs (8, 9, 14). However, umbilical cord blood (UCB) has become an attractive source of stem cells, because of its noninvasive collection procedure and rapid availability from cord blood banking (17, 18). Human UCB-derived MSCs (hUCB-MSCs) exhibit higher proliferation capacity and lower immunogenicity compared with BM-MSCs (17, 19). Data from a few reports support that UCB-MSCs may have greater immunosuppressive potential than other sources of MSCs (17–22). In addition, hUCB-MSCs have shown greater immunosuppressive and regenerative potential than BM- or peripheral blood–derived MSCs in murine wounding model (23). A preclinical study has demonstrated that repeated systemic infusions of human UCB-derived unrestricted somatic stem cells, a subpopulation of nonhematopoietic stromal stem cells, significantly extended the life span and reduced blistering in a RDEB mouse model (16). Given the promising results of the preclinical study, we conducted a first-in-human, phase I/IIa clinical trial of intravenous administrations of allogeneic hUCB-MSCs in patients with RDEB to determine safety, tolerability, and potential efficacy. We also analyzed changes in serum inflammatory markers, neuropeptides, and skin inflammatory infiltrates as well as C7 expression following hUCB-MSC treatment.
Patient characteristics. Between October 2016 and May 2019, 6 patients with RDEB were assessed for eligibility. Three adult and two pediatric patients were sequentially enrolled in the trial and received 3 repeated intravenous hUCB-MSC injections. One additional adult patient was treated with the same investigational product under the treatment use approval from the Korea Food & Drug Administration (KFDA), because they were too late for trial enrollment (Figure 1). All patients had moderate-to-severe or severe phenotypes, with various extracutaneous symptoms. Negative or markedly decreased expression of C7 noncollagenous-1 domain was found in baseline skin biopsies. Analysis of circulating autoantibodies against C7 using indirect immunofluorescence (IIF) was negative for all patients (Table 1). All adult patients received 3 × 106 hUCB-MSCs/kg every 2 weeks, whereas the 2 pediatric patients received 1 × 106 to 2 × 106 hUCB-MSCs/kg every 2 weeks. All patients were carefully observed for clinical signs and laboratory test results related to potential thromboembolic events were monitored, even though a recent meta-analysis of randomized controlled trials reported no significant increase in the risk of thromboembolic events for patients treated with MSCs as compared with the control group (24). Demographics and clinical characteristics of participants and trial flow are provided in Figure 1 and Table 1. All patients completed at least 8 months (8–24 months) of follow-up after the first infusion.
READ MORE: https://insight.jci.org/articles/view/143606
